Living with a bleeding disorder
From managing bleeds and joint health to finding ways to stay active—living with a bleeding disorder can come with challenges.
Explore these everyday tips, tools, and strategies to help you plan for some of those challenges.
Leandro lives with hemophilia A.
Growing up with a bleeding disorder
Abdul lives with hemophilia A.
From spotting early bleeds to helping kids stay active and prepared, childhood brings unique challenges. Explore tools and resources designed just for families and caregivers.
Bleed management can mean healthier joints
Joint bleeds, also called hemarthrosis, can cause lasting damage—joint bleeds are especially likely in knees, elbows, and ankles. Bleeds may lead to swelling, pain, and tightness in the joints. High-quality medical care from knowledgeable healthcare providers can help protect joint health.
Actor portrayal
Treating bleeds fast
Being prepared and knowing what to look for means faster bleed care. Know the signs, act quickly, and work with your care team to create a plan that helps you manage bleeds when time matters.
Signs of an internal bleed
Bleeds can happen inside joints or muscles, not just from cuts or injuries. Internal bleeds aren’t always easy to see—know what to look for:
- Swelling, warmth, or bruising
- Tingling, tightness, or pain
- Stiffness or reduced movement
- Weakness of balance issues
- Headache or dizziness
Leandro lives with hemophilia A.
- Not able to walk properly
- Headache
- Feeling dizzy
- Feeling very sleepy
- Blurry vision
- Weak or sore arms or legs
- Trouble with urination or bowel movements
- Red or black stool
- Red or black vomit (may look like coffee grounds)
- Tingling in joint
- Tightness in joint
- Warmth
- Swelling, larger than the other joint
- Gradual increase in pain if untreated
- Pain, especially when bending
- Limping, especially in children
- Tightness in muscle
- Warmth
- Swelling
- Not able to move your arm or leg properly
- Limping
- Pain, especially when walking
Important safety note:
Bleeds in the head, neck, spine, or stomach are particularly serious.
Contact your doctor immediately if you have symptoms in these areas.
Joint health
Bleeds can occur in or near joints like the ankles, knees, elbows, and hips. The sooner you treat, the better—early treatment can help stop pain, control bleeding, and prevent recurrent bleeding or a more serious bleed that is difficult to control.
Take action to protect your joints:
- Treat as soon as possible after noticing symptoms
- Don’t wait for pain or limited movement to act
- Create an action plan with your HTC
- Report any joint changes to your doctor right away
Stay Active
Staying active, managing your weight, and following your doctor’s advice can all help protect your joints.
Check out our tips for staying active—safely.
Experiencing reduced mobility?
You're not alone.
Actor portrayal
Experiencing reduced mobility? You’re not alone.
In the HERO Study by Novo Nordisk,
59%
of adults with hemophilia reported limited mobility.
The HERO study asked 675 adults with hemophilia from 10 countries to fill out a health survey about their daily life, including questions about mobility, self-care, daily activities, pain/discomfort, and anxiety/depression. The answers were combined into a single score to help understand how hemophilia affects quality of life. Because the study was based on people’s own reports at one point in time, it may not capture every experience or show cause and effect.
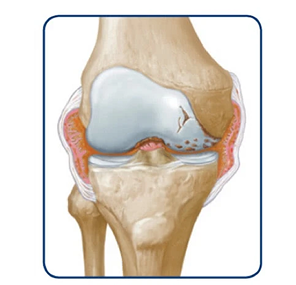
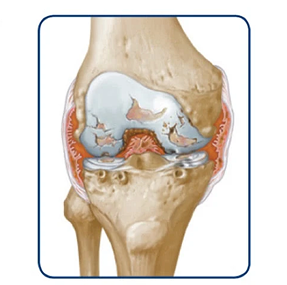
Joint bleeds—also called hemarthrosis—can happen when a joint is stressed. Repeated bleeds in the same joint may lead to chronic synovitis, where the joint lining becomes swollen and thick. Over time, this can limit movement and cause lasting joint damage.
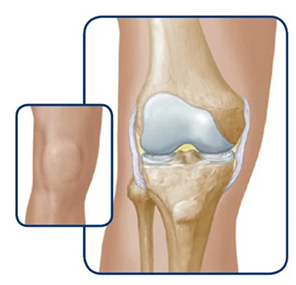
Healthy knee
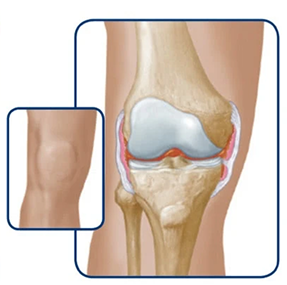
The bleed starts to enter the joint
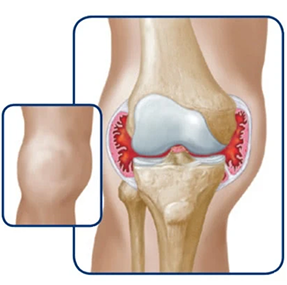
The joint swells
If bleeds continue, it can degrade the cartilage and bone within the joint.
Over time, the joint may swell, change shape, and lose mobility.
Once a joint is severely damaged, it may not heal on its own. You could lose range of motion or develop a fixed joint that no longer moves. When joint damage becomes permanent, it’s called hemophilic arthropathy. Discuss treatment options with your doctor before the joint damage becomes permanent. Treatment options may include surgery.
Swelling of tissues in the knee may become permanent
Over time, this can lead to wearing away of the bone
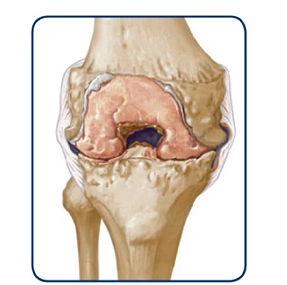
Permanent damage results in a destroyed joint
Considering joint surgery?
For some people with a bleeding disorder, surgery can relieve pain and improve mobility when joints are damaged. It’s a personal decision—one to make with your doctor and family.
Surgery can help—but it comes with risks. Talk with your doctor about whether it’s the right step for you.
Ask yourself:
- How often do joint issues affect your daily life?
- How much pain are you in?
- Do you have insurance coverage?
- Can you commit to physical therapy?
- What are your personal goals?
Pain and hemophilia: What you should know
Let’s take a closer look at the different types of pain—and how to manage them when they show up.
The HERO Study explored how hemophilia affects daily life. One major finding: pain is a constant for many who have hemophilia.
reported pain recently
interfered with their daily life
reported living with persistent paina
a21% reported persistent pain and 29% reported persistent pain that worsens when they have a bleed.
The HERO study asked 675 adults with hemophilia from 10 countries to fill out a health survey about their daily life, including questions about mobility, self-care, daily activities, pain/discomfort, and anxiety/depression. The answers were combined into a single score to help understand how hemophilia affects quality of life. Because the study was based on people’s own reports at one point in time, it may not capture every experience or show cause and effect.
Acute vs. chronic pain:
what’s the difference?
Acute Pain
Acute pain comes on suddenly, is usually intense, and can last hours to days. In hemophilia, it’s often a sign of a joint or muscle bleed.
Chronic Pain
Chronic pain lasts for months or longer. It can be caused by repeated bleeds or long-term joint damage.
Common symptoms
- Tingling
- Swelling
- Warmth in the joint
- Decreased range of motion
- Pain that lasts for months or more
- Joint stiffness or severely limited movement
Likely cause
- A bleeding episode in joints and/or muscles
- Ongoing joint damage
- Effects of repeated bleeds over time
IF ignored
- Slower recovery
- Risk of joint damage and chronic pain
- Increased difficulty moving joints
- Trouble with daily tasks
What helps
- Factor treatment
- R.I.C.E. (Rest, Ice, Compression, Elevation)
- Approved pain medication
- Approved pain medication
- Stretching or exercise
- Physical therapy
Avoid
- Ignoring the pain
- Medications that inhibit clotting (ask your care team)
- Not using or moving the joint
- Ignoring chronic pain
- Medications that affect clotting
Note
Bleeding patterns can vary widely—even within the same severity level. Talk to your care team about what’s typical for you.
Managing your pain
The first step in managing pain from a joint bleed is treating bleeds early. The sooner you are able to treat a bleed, the better your chances of stopping the bleed and protecting your joints.
Start pain management at the first signs of a joint bleed to:
Relieve short-term pain
Reduce the risk of long-term damage
R.I.C.E. can help reduce pain and swelling after a joint bleed.
Administer your prescribed factor and contact your HTC if needed.
Use the R.I.C.E. method:
Limit use of the joint for at least 24 hours
Apply cold packs for 15–20 minutes
Use a wrap or bandage (not too tight)
Raise the joint to reduce pressure and swelling
Brian lives with Factor 8 deficiency.
Keep moving to help manage pain
Gentle movement and safe exercise can help relieve
pain and protect your joints. For people living with a bleeding disorder, staying active can support mobility and reduce stiffness—adding movement may improve overall function and help you regain and maintain functional independence.
Work with your care team and a physical therapist to create
a daily exercise plan that’s right for you.
Check out our tips for staying active—safely.
Remember
Bleeds can hurt—chronic bleeds may cause joints to swell and lose motion. That can lead to lasting joint damage, which may mean more pain and less mobility over time.
Planning for the unexpected
When you are living with a bleeding disorder, a little preparation today can make a big difference in an emergency.
Actor Portrayal
Tip
Call your HTC or doctor on the way to the ER—they may help speed things up once you arrive.
Register with your local hemophilia treatment center (HTC).
Your HTC can coordinate with ER staff during an emergency.
Ask which local ERs are best equipped.
Some hospitals have on-call hematologists or “fast tracks” for patients with serious conditions.
Request an emergency letter from your doctor.
Request a letter from your doctor or your child's doctor that includes their type and severity of hemophilia, inhibitor status, medications, and treatment plan. Carry copies with you and keep one in your go-bag.
Pack a go-bag in advance.
Include:
- All necessary medications and supplies
(eg, factor infusion kit)
- Ice packs and safe pain relievers recommended by your doctor
- Emergency letter and medical history
When to head to the ER
Not sure if it’s an emergency? Your doctor or HTC can help you decide.
According to The National Bleeding Disorders Foundation, some common reasons to head to the ER include if you:
Have a head or stomach injury
See blood in stool or are vomiting blood
Experience numbness in an arm or leg
Have a deep cut or laceration
Or if you’re unable to reach your HTC and you need treatment.
To learn more, go to the National Bleeding Disorders Foundation.
Medical or dental procedures
Before any planned surgery or dental work, let your care team know about your bleeding disorder—even small procedures can lead to prolonged bleeding. Your HTC can help you coordinate the right care.
Good oral health is essential for people with hemophilia
Prevent problems and reduce risks of dental complications by focusing on regular, preventive care.
Finding the right dentist
Look for a dentist experienced with bleeding disorders. Ask directly before scheduling an appointment, and if you're unsure where to start, your HTC, local NBDF chapter, or hemophilia community can help with referrals. Hospital-based dental clinics may also offer specialized care.
Plan ahead for oral surgery
Before oral surgery—like extractions or implants—talk to your HTC or hematologist and dentist. They can help coordinate a care plan to consider potential complications.
Preparing for a Trip
For people with hemophilia, smart travel starts with planning ahead and knowing how to handle a bleed.
Do you know where the hemophilia treatment centers (HTCs) and hospitals closest to your destination are?
Check the list at the Centers for Disease Control and Prevention.
- Pack copies of prescriptions and medication labels
- Check your health insurance for travel coverage
- Consider wearing a medical ID emblem if traveling alone to help inform medical personnel if you become unconscious or unable to communicate during an emergency.
- Build in extra time for travel if using a stroller, wheelchair, or crutches
- Bring extra factor and supplies
- Consider wearing a medical ID emblem if traveling alone to help inform medical personnel if you become unconscious or unable to communicate during an emergency.
- Know where the closest HTCs are at your destination
- Carry your insurance card and any important medical documents
- Keep medicine in your carry-on—not in checked bags
- Get a letter from your doctor or HTC explaining your medical supplies
- Arrive early, especially if you have mobility needs
- Request a seat with extra legroom if needed
- Review TSA guidelines for medications and mobility devices at tsa.gov
Safety first!
Staying active with hemophilia
Exercise isn’t off-limits for people living with hemophilia. In fact, it’s encouraged. Staying active can help strengthen muscles, protect joints, and maintain a healthy weight, all of which can reduce stress on the body. Just be sure to choose activities that are right for you or your child and talk to your care team first.
Dolvett Quince–celebrity fitness expert.
Looking for guided workouts?
Get Fit. Stay Fit. With H-Fit. Led by celebrity trainer Dolvett Quince. Explore joint-friendly exercises and feel-good routines you can do at home.
Staying active: understanding activity risks
Physical activity is important when living with a bleeding disorder, but different activities carry different levels of risk.
Here’s where common activities typically fall:
Brian lives with Factor XIII deficiency.
These are generally safe activities, often with minimal bleeding risk:
- Aquatics and swimming
- Archery
- Golf
- Tai Chi
- Walking
These activities may be appropriate with certain precautions, factor coverage, or supervision:
- Bowling
- Jumping Rope
- Running or Jogging
- Cross-country skiing
- Tennis
These activities often have a higher risk of injury and may require careful planning or avoidance:
- Boxing
- Tackle football
- Power lifting
- Rugby
- Wrestling
Remember: These examples are for informational purposes only—not recommendations. Always consult your care team to decide what’s right for you.
Playing it safe:
A guide to physical activities.
Learn more about the risks and benefits of physical activities in the National Bleeding Disorders Foundation’s Playing It Safe guide.
Are you making trade-offs by compromising on bleed protection or ease of administration?
Nikola lives with hemophilia A.
Are you speaking your truth about managing your hemophilia A?

