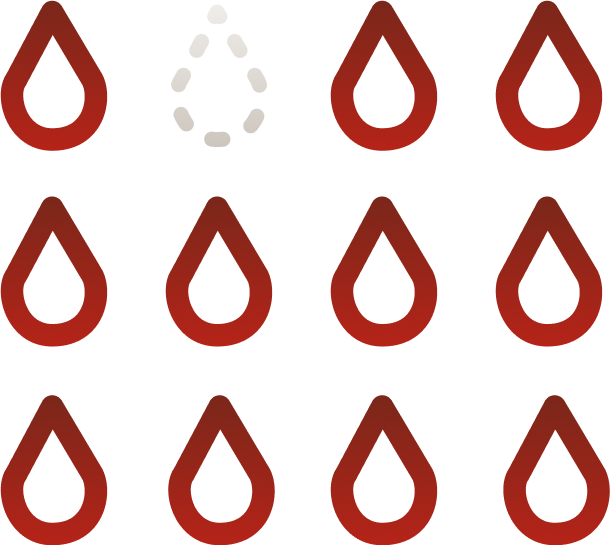
The two main types of hemophilia
Hemophilia is a bleeding disorder caused by low levels of clotting factor in the blood. While there are many types of bleeding disorders, hemophilia usually refers to these two:
Hemophilia A
Caused by low levels of clotting Factor VIII
About 80% of people with hemophilia have this type.
Hemophilia B
Caused by low levels of clotting Factor IX
It affects the remaining 20%